- Bulletin: Summer 2025
- Training and careers
Collaborative Effort for Patient Outcome Development (CEPOD)
MMH tell us about their very successful quality-improvement project.
Authors:
- Dr Ishan Wijesinghe, Registrar Anaesthetics, Medway Maritime NHS Foundation Trust
- Dr A C Ruwanmali De Silva, Consultant Anaesthetist, Medway Maritime NHS Foundation Trust
We’re very proud that Medway Maritime Hospital's CEPOD team recently achieved notable recognition for their quality-improvement project with the highly commended prestigious national HSJ Award. This accolade highlights the innovative efforts aimed at enhancing patient safety and outcomes in emergency surgical care.
Dedicated operating theatres for emergency surgery, often referred to as CEPOD theatres, were introduced in the early 1990s to enhance the quality and safety of emergency surgical care. However, the efficient use of CEPOD theatres remains a persistent challenge. The process of ensuring that emergency patients are taken to the theatre promptly and safely is highly complex and depends on a multitude of factors. Our project at Medway Maritime Hospital sought to identify specific inefficiencies within this process and aimed to implement targeted improvements to optimise the utilisation of theatre time.
We conducted our quality-improvement project in two phases. The first phase involved data collection over a one-month period in September 2022, focusing on 95 patients who underwent surgery in the CEPOD theatre. Data was collected daily between 8am and 6pm, including weekends. Key information gathered included the time of booking, time of surgery, CEPOD category, and details on delays such as their length and reasons. The preparation steps evaluated included the readiness of the surgeon, anaesthetist, and ward staff, as well as the team briefing, patient transfer, and arrival at the CEPOD theatre in a timely manner.
Out of the 95 patients, data was missing for three, leaving 92 cases for analysis. Delays in one or more preparation steps were identified in 66.4% of cases. Among the 46 patients classified under the ‘urgent’ category, requiring surgery within 2–6 hours, the target timeframe was met in only 44% of cases. The median waiting times were one hour for immediate surgery, seven hours and seven minutes for urgent surgery, and 15 hours for expedited surgery. A recurring pattern was observed where one delay triggered subsequent delays in the process, highlighting inefficiencies that amplified over time and contributed to prolonged wait times for patients. These findings were shared with all teams involved, including theatre staff.
The action plan included the following measures:
- Reinforcing the 8am CEPOD theatre ‘huddle’, where surgical specialties collaboratively discuss their listed patients and agree on the order of procedures.
- Implementation of a transparent, remotely accessible electronic booking system.
- Establishment of a ‘golden-patient’ protocol, ensuring that one patient is fully prepared the previous day to be first on the list.
- Development of a pre-surgery checklist to ensure all necessary preparations are completed for each patient for ‘ward readiness’.
- Identification of designated leads from all surgical and anaesthetic teams to oversee and drive progress. Team meets monthly.
- Identifying and training two emergency surgery facilitators to make sure patients are ready to arrive in the theatre.
- Improved results by engaging and promoting collaborative decision-making across teams.
- Celebrating good work on a gratitude board.
- Encouraging a shift in work culture, allowing CEPOD cases to be accommodated during gaps created by cancellations in the elective theatre lists.
These interventions are aimed at streamlining processes, reducing delays, and optimising the use of CEPOD theatre time, fostering a more coordinated and efficient workflow. It is also important to highlight that the interventions were implemented using existing resources, and that no additional funding was required. We were able to align after-midnight operations with national standards due to enhanced daytime efficiency, providing better learning opportunities.
Following the implementation of the above interventions, data collection for Phase 2 was conducted from 2 October to 31 October 2023. Data was collected using the same methodology as in Phase 1.
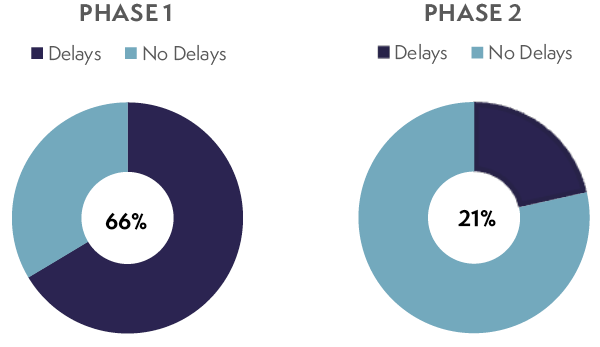
The dataset included 145 patients, with one case excluded due to incomplete data, leaving 144 cases for analysis. The total number of cases increased by 52.6% compared to the 92 cases in Phase 1. Delays were identified in 21.5% of cases, a significant improvement from 66.4% (Figure 1) in the first phase. In terms of breaches of CEPOD category time-targets, 15.1% of urgent cases and 27% of expedited cases exceeded the recommended timeframes in Phase 2. This marks an improvement compared to Phase 1, where 43.5% of urgent cases and 29.7% of expedited cases breached the target times.
Figure 1: Analysis of delays in all CEPOD theatre cases
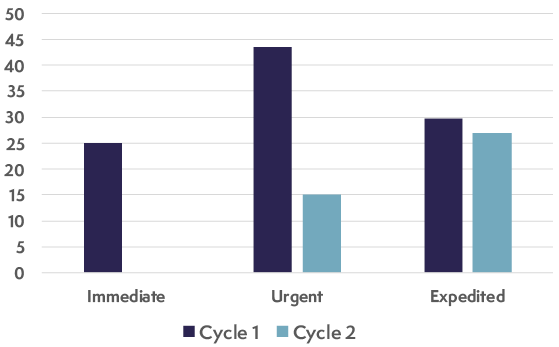
Furthermore, all seven ‘immediate’ cases commenced within one hour, which is a notable improvement from the 25% delay observed previously. Delays were significantly reduced in Phase 2, with only 27.3% of urgent cases and 21% of expedited cases experiencing delays (Figure 2). This represents a marked improvement compared to Phase 1. The median waiting time for urgent surgeries decreased from seven hours to one hour, highlighting the effectiveness of the implemented interventions.
Figure 2: Analysis of breaches across all CEPOD categories
Further improvements focused on categorising patients correctly under CEPOD, getting active input from on-call consultants, and fostering a culture of change through rewards.
The third phase of re-auditing has just been completed, mainly to ascertain compliance of systems that are in place, to identify further gaps and to further foster collaborative working culture. Efficiency has dropped slightly compared to the second cycle. However, this has given us a good insight into where reinforcement is required and has led to the introduction of more clarity by means of standard operating procedures where required. Ongoing audits are required not only to keep the standards, but also to identify and introduce new strategies to further improve patient care. We are in the process of reaching out to create a regional network to share best practice.