Risks and side effects – sore throat
Translations are available for this leaflet.
About this leaflet
This leaflet is about having a sore throat after a general anaesthetic. This is a side effect that you might experience if you have a general anaesthetic. It explains the causes of a sore throat and what can be done about it.
General anaesthetics are medicines that give a deep sleep-like state. They are essential for some operations and procedures. During a general anaesthetic you are unconscious and feel nothing.
You can read about different types of anaesthetics in our Patient information leaflets and video resources section.
What does it feel like?
- You might have some discomfort or more severe pain in your throat.
- A sore throat usually lasts for 24–48 hours.
- Your voice might be hoarse.
- Your throat might feel very dry.
How likely is it to happen?
How likely it is depends on the equipment that your anaesthetist uses.
Out of every 100 people
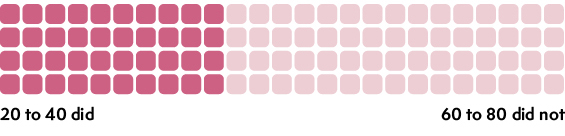
These numbers come from research studies. You can find out about the research we used in our Anaesthesia and risk evidence table.
What causes a sore throat after anaesthesia?
Some anaesthetic gases and medicines can make your throat dry.
Some of the equipment that anaesthetists use during a general anaesthetic can irritate your throat.
During a general anaesthetic, the muscles in your body relax, including those around your throat and chest. This can reduce the amount of air that gets into your lungs.
To ensure a continuous flow of oxygen to your lungs, the anaesthetist may place a breathing tube in your throat to keep your airway open. They usually do this after you are unconscious.
Tubes or masks that your anaesthetist uses while you are unconscious can give you a sore throat because:
- they can irritate your throat when they are put in or removed
- some are inflatable and can press on your throat when they inflate. This can cause discomfort.
More information can be found in our leaflet Your airway and breathing during anaesthesia.
What can help?
You can use pain relief such as ibuprofen or paracetamol. You should check with your GP or pharmacist which pain relief is best for you. Your hospital may also give you some pain medicine before you go home.
When to seek help
If the pain worsens and you have trouble swallowing one week after the anaesthetic, you should see your GP or nurse or seek advice from a pharmacy.
If, at any time, you are having any difficulty breathing or cough up blood, you should contact your GP or your anaesthetist urgently for further advice.
This leaflet has been produced by Leila Finikarides for the RCoA, in collaboration with patients, anaesthetists and patient representatives of the RCoA.
Disclaimer
We try very hard to keep the information in this leaflet accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this leaflet as a guide. This leaflet on its own should not be treated as advice. It cannot be used for any commercial or business purpose. For full details, please click here.
Sixth Edition, November 2024
This leaflet will be reviewed within three years of the date of publication.
© 2024 Royal College of Anaesthetists
This leaflet may be copied for the purpose of producing patient information materials. Please quote this original source. If you wish to use part of this leaflet in another publication, suitable acknowledgement must be given and the logos, branding, images and icons removed. For more information, please contact us.