Your airway and breathing during anaesthesia
Translations are available for this leaflet.
This leaflet explains why and how the anaesthetist manages your airway and breathing during anaesthesia.
Contents
- What is the airway.
- Why it is necessary to manage your airway during an operation.
- How your airway is assessed before surgery.
- How your airway is managed during an operation.
- Risk and shared decision-making.
Your airway and breathing
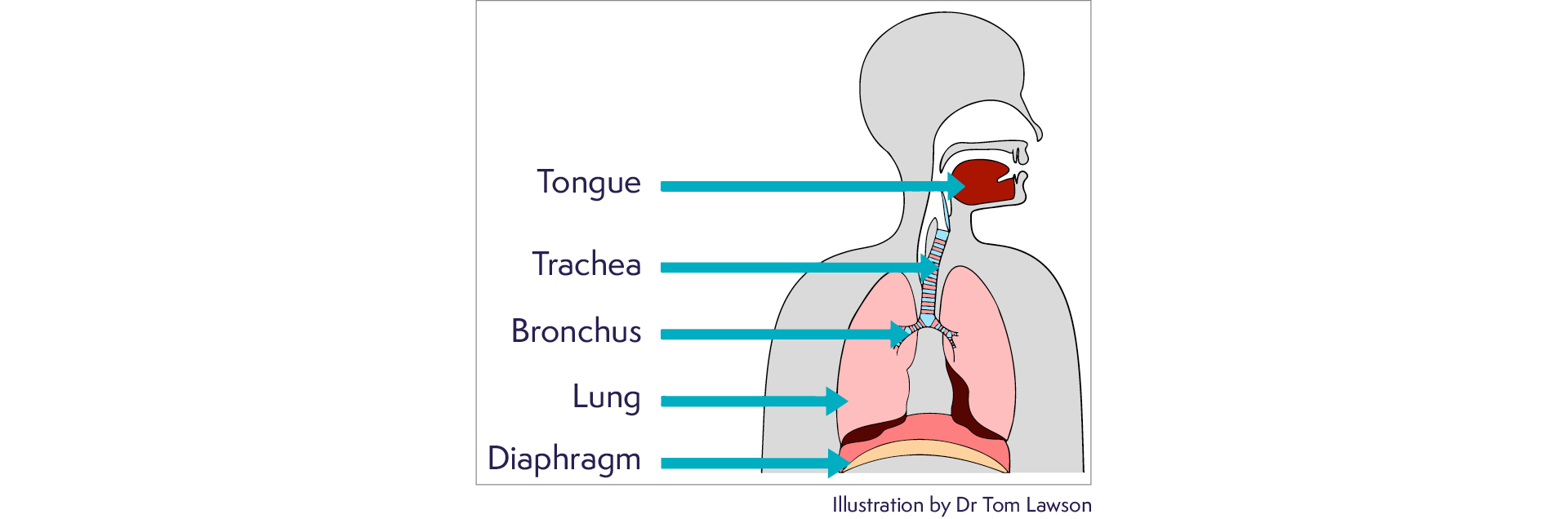
As you breathe, air enters through your nose and mouth and flows down through your throat and larynx (voice box) into the trachea (windpipe) to reach your lungs. The combination of these structures is commonly referred to as the ‘airway’. Your body takes the oxygen that it needs from this air.
Getting oxygen to your lungs during anaesthesia
(managing your airway)
Making sure that oxygen can continue to flow through your airway and to your lungs is a vital part of having a general anaesthetic. Anaesthetists are trained to assess your airway and manage your breathing during anaesthesia. They are also responsible for looking after you during the anaesthetic, and ensure that you are safe at all times and wake up comfortably.
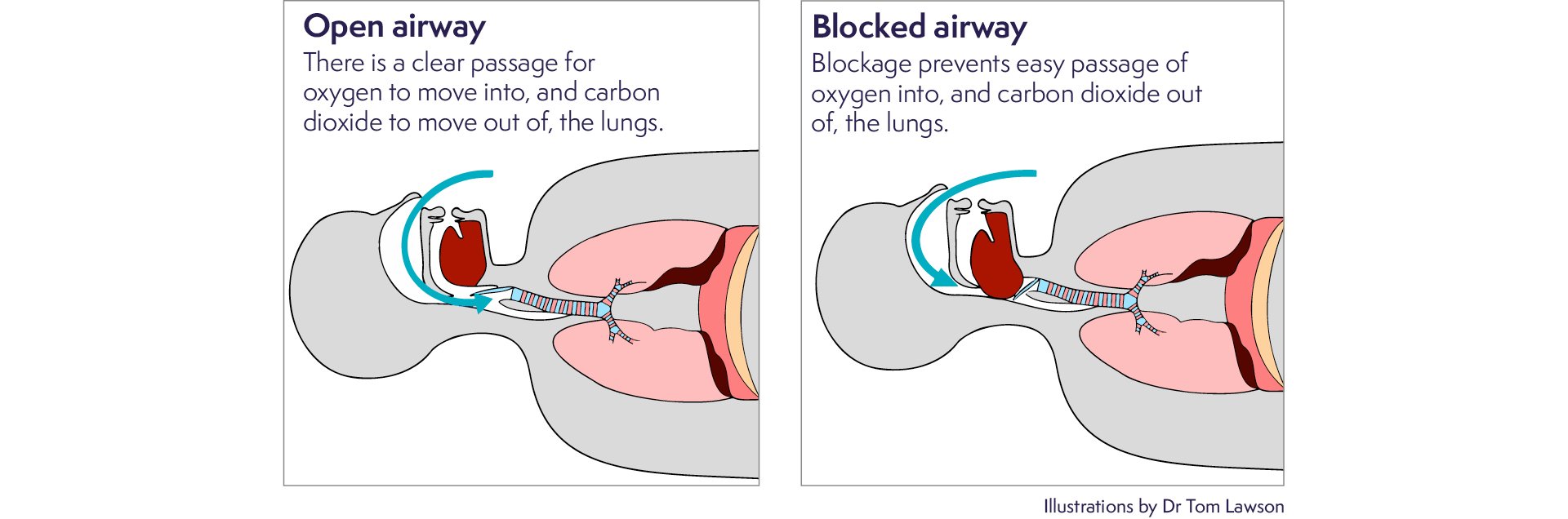
During a general anaesthetic, the muscles in your body relax, including those around your throat and chest. This can lead to your airway becoming blocked or your breathing becoming restricted. To ensure a continuous flow of oxygen to your lungs, the anaesthetist may place a tube into your trachea to keep your airway open – this is called tracheal intubation.
It is common practice for the tube to be inserted after the anaesthetic has been given and once you are asleep, so that you will have no awareness of this procedure.
There are some instances when it is safer to have an ‘awake tracheal intubation’, where the tube is placed in your trachea before the anaesthetic drugs have been given. You can find out more information about awake tracheal intubation on the Difficult Airway Society (DAS) website.
The anaesthetist will discuss with you the method that they think is safest for you. In the vast majority of cases intubation is done while the patient is asleep.
For more information on anaesthesia in general and different types of anaesthetics, please read the RCoA leaflet: You and your anaesthetic.
How your airway is assessed before surgery
Anaesthetists need to assess you and your airway so that they can plan the safest way to manage your anaesthetic. They will ask you some general questions about any relevant medical conditions and previous anaesthetics that you may have had. They will check whether you have any conditions that might prevent you from moving your neck freely. They will also check whether you have any issues with opening your mouth fully, any problems with acid reflux or any significant dental work. If you have a growth or swelling in your airway or neck, the anaesthetist will look at any relevant ultrasound or CT (computed tomography) scans as part of their assessment.
The anaesthetist will ask you to perform a few simple tests to see:
- whether you can open your mouth widely and if they can see the back of your throat easily
- how your jaw moves by asking you to move your bottom jaw or bite your top lip
- whether you can move your neck through a range of movements and simple exercises.
Occasionally, they might need to look into your nose using a small flexible camera – this is a painless procedure.
If you have previously been told about any difficulties in managing your airway and breathing, it is important that you inform the anaesthetist. The anaesthetist might need to look at any records from your previous anaesthetics if they are available.
Before the general anaesthetic starts, you will be asked to breathe oxygen either from a plastic facemask or through soft plastic tubes placed at the entrance to your nose. This boosts the amount of oxygen in your lungs.
What if there are difficulties managing my airway?
If your airway will require specific management for future anaesthetics, the anaesthetist may (with your consent) enter your details into the DAS Difficult Airway Registry. This way If you require an anaesthetic in the future, you can let the anaesthetist know that you are registered with the DAS Registry and they will be able to look up your details to help them plan the safest anaesthetic for you. Information about the Registry can be found on the DAS website.
You may also wish to wear an alert bracelet in case you require emergency surgery and are not able to communicate with the hospital staff.
Risk and shared decision-making
Modern anaesthetics are very safe. There are some common side effects from the anaesthetic or equipment used, including equipment used to manage your airway. These are usually not serious or long lasting.
You can read more detail about minor risks associated with anaesthesia here.
There are more serious risks associated with managing a patient’s airway, although these are uncommon, rare or very rare. A large study on complications of airway management has found that one major airway complication occurs for every 22,000 general anaesthetics. This is the equivalent of one person in a small town.
However, your specific risks will depend on your physical condition and the type of surgery that you are having. Your anaesthetist will discuss with you the risks that they believe to be more significant for you.
Complications associated with managing a patient’s airway include the following.
Failed intubation
Sometimes the anaesthetist may initially find it difficult or even impossible to place the tube into your trachea This is known as a ‘failed intubation’. The anaesthetist may decide that it is safer to wake you up and postpone your surgery. Alternatively, they may decide to use a different method from a range of techniques available for inserting the airway. Failed intubation is uncommon, but is, however, more common in women who are pregnant in emergency situations and for patients requiring emergency surgery with a general anaesthetic.
Aspiration
On rare occasions there may be serious complications as a result of problems with a patient’s airway. This can be caused by stomach contents going into the lungs, and is known as aspiration.
Very rarely, serious airway complications may lead to an unexpected admission to intensive care, brain damage or death.
What you can do to reduce your risk
Fitness and lifestyle
Fitter patients who are able to improve their health and lifestyle recover from surgery more quickly and with fewer complications.
There is much you can do to prepare yourself for an operation. Even small changes can make a big difference. You might want to increase your levels of physical activity and improve your diet. If you drink or smoke, you should consider cutting back or even stopping.
If you have a long-standing medical problem, it might be a good idea to check with your GP surgery whether there is anything that you can do to improve it well ahead of the surgery.
If you have obesity or are overweight, this can make it more difficult for the anaesthetist to manage your airway and you might want to try to reduce your weight ahead of the surgery.
Our Fitter Better Sooner resources will provide you with the information that you need to become fitter and better prepared for your operation.
Teeth
It is very important that you tell the anaesthetist about any significant dental work or damage to your teeth. You may want to consider a visit to the dentist ahead of your surgery.
Fasting and pre-medication
The hospital should give you clear instructions about when to stop eating and drinking. These instructions are important. If there is food or liquid in your stomach during your anaesthetic, it could come up into your throat and lungs and endanger your life. Some hospitals will allow you to ‘sip til send’ if appropriate. This means that you will be allowed to drink small amounts of clear liquids right until the time of your surgery to help you stay hydrated. You can read more about ‘sip til send’ on the Centre for Perioperative Care’ website.
Obstructive sleep apnoea
If you have obstructive sleep apnoea, you are more at risk of airway difficulties. You may need to have an overnight stay after your surgery and you will be closely monitored after your anaesthetic. If you have a CPAP (continuous positive airway pressure) machine, you should bring it with you.
Beards/facial hair
The anaesthetist needs to use a close-fitting facemask to provide oxygen. Thick beards can prevent these from fitting snugly as they should. The anaesthetist will discuss with you if they think there is a risk of the mask not working properly and what the options might be.
Hairstyles/hair extensions
The anaesthetist needs to be able to move your neck freely to have safe access to your airway. It is advisable to remove large volumes of hair extensions before having an anaesthetic, because these can restrict movement in your neck.
Shared decision-making
Shared decision-making ensures that individuals are supported to make decisions that are right for them. It is a collaborative process through which a clinician supports a patient to reach a decision about their treatment.
The conversation brings together:
- the clinician’s expertise, such as treatment options, evidence, risks and benefits
- what the patient knows best: their preferences, personal circumstances, goals, values and beliefs.
Find out more on the National Institute for Health and Care Excellence website.
Below are some tools that you can use to make the most of your discussions with your anaesthetist or preoperative assessment staff:
- Choosing Wisely UK BRAN framework – use this as a reminder to ask questions about treatment
- NHS ask three questions – there may be choices to make about your healthcare
- Centre for Perioperative Care (CPOC) – CPOC has produced an animation to explain shared decision-making.
Questions you might like to ask
If you have questions about your anaesthetic, write them down (you can use the examples below and add your own). If you want to speak to an anaesthetist before the day of your operation, contact the preoperative assessment team who may be able to arrange for you to speak to an anaesthetist on the telephone or see them in a clinic.
- Are there any issues with my airway?
- Do I have any special risks?
Disclaimer
We try very hard to keep the information in this leaflet accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this leaflet as a guide. This leaflet on its own should not be treated as advice. It cannot be used for any commercial or business purpose. For full details, please click here.
Second Edition, October 2023
This leaflet will be reviewed within three years of the date of publication.
© 2023 Royal College of Anaesthetists
This leaflet may be copied for the purpose of producing patient information materials. Please quote this original source. If you wish to use part of this leaflet in another publication, suitable acknowledgement must be given and the logos, branding, images and icons removed. For more information, please contact us.