View from the frontline of anaesthesia during COVID-19, April 2020 survey results
View from the frontline of anaesthesia during COVID-19
Over a 24-hour period from 15-16 April 2020, the College conducted a survey to develop a snapshot ‘view from the frontline’ of anaesthesia during COVID-19.
Introduction
16% of all hospital consultants are anaesthetists, making anaesthesia the single largest hospital specialty in the UK. Anaesthetists of all grades play a critical role in the care of two-thirds of hospital patients. 2,174 members completed the survey. This briefing presents the findings and a detailed picture of the issues faced by anaesthetists across the UK.
Who is this briefing for?
College fellows and members, clinical directors, civil servants, ministers, parliamentarians, NHS, public health and social care organisations across the UK, our partners, and the public.
What is this briefing for?
To represent the voice of the College’s members on the issues that matter most to them during COVID-19, and to feedback their views as expressed in the COVID-19 survey.
To support civil servants, ministers, parliamentarians and key decision makers to understand, and mitigate, the pressures faced by anaesthetists during COVID-19 as they care for their patients.
To highlight the indispensable role of anaesthetic teams in fighting COVID-19, and to encourage decision-makers and the public to champion the profession.
Key findings
- 17% of respondents have or are currently taking time off work because of suspected COVID-19, rising to nearly a quarter when including confirmed cases of COVID-19.
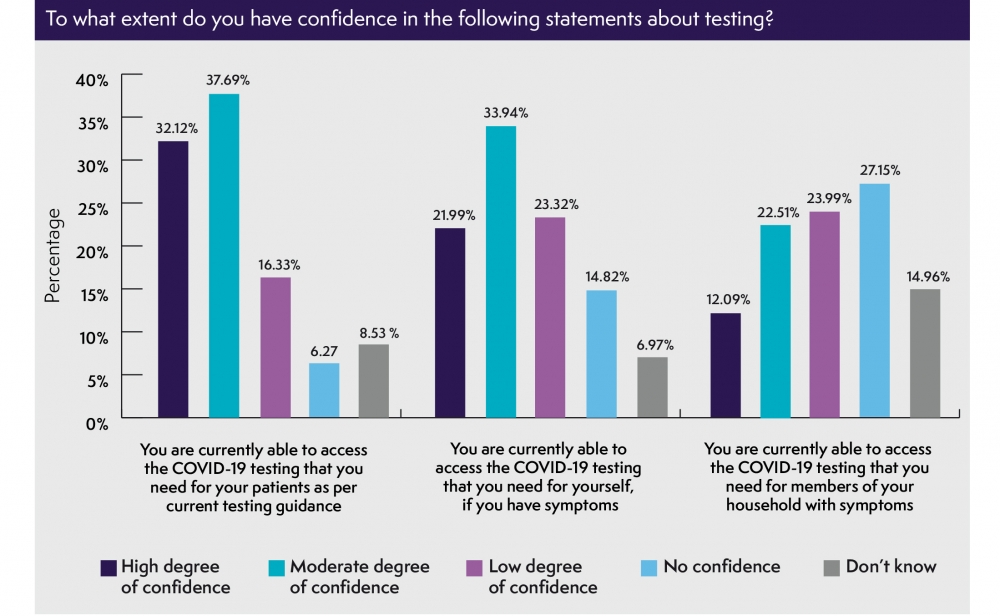
- Nearly 40% of respondents are unable to access the testing they need for themselves, while over 50% don’t have the testing they need for household members, and one in five are unable to access the testing they need for their patients.
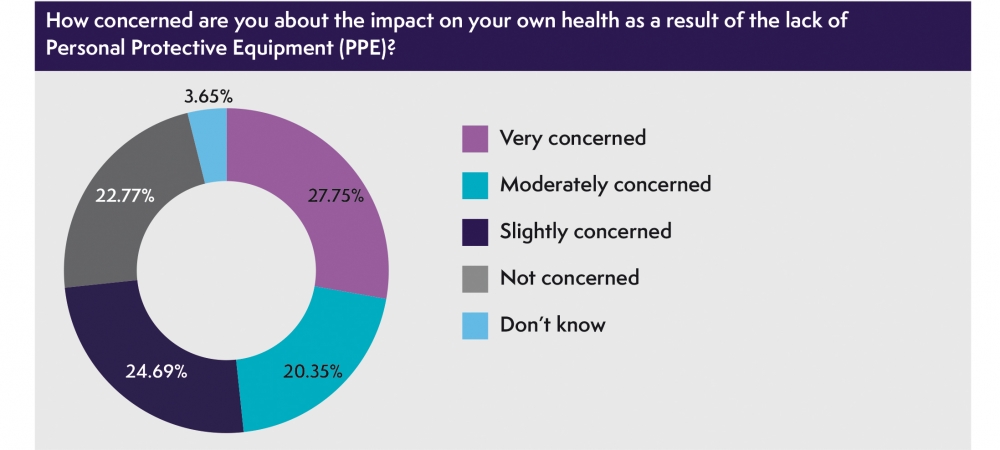
- Over two thirds of respondents 73% told us they feel concerned for their health because of a lack of adequate PPE, with nearly one third 28% very concerned, while over one quarter feel pressurised to treat patients without adequate PPE and nearly 17% are unable to access the PPE they need.
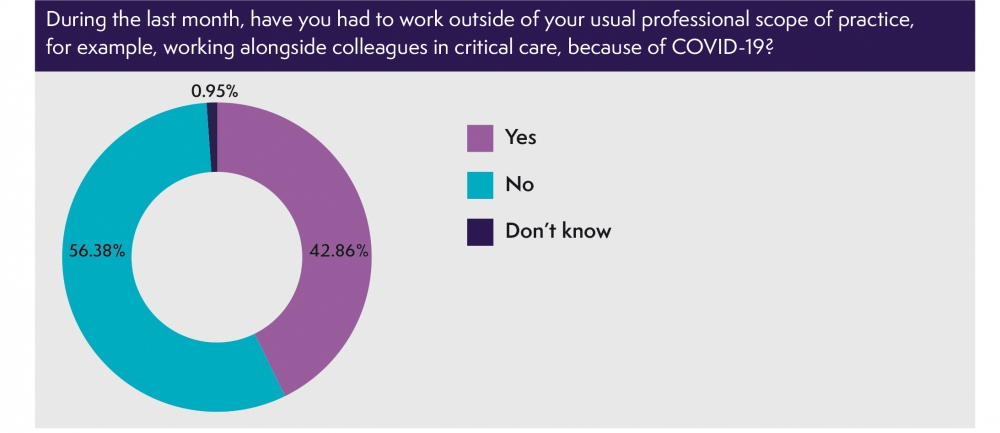
- Over four in ten of respondents have worked outside of their usual area of practice during the last month
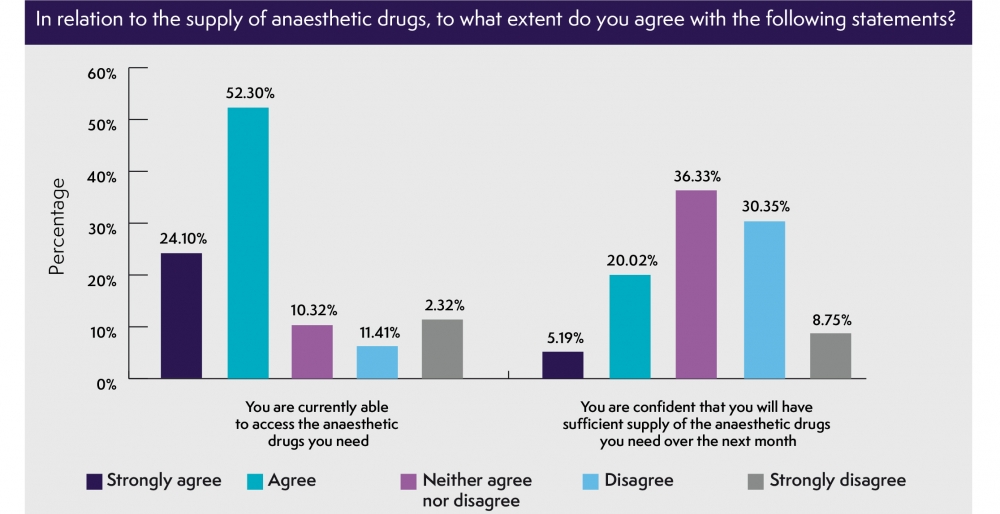
- One in ten respondents can’t currently access all the usual anaesthetic drugs they use for their patients; 40% aren’t confident they will have sufficient supply over the next month.
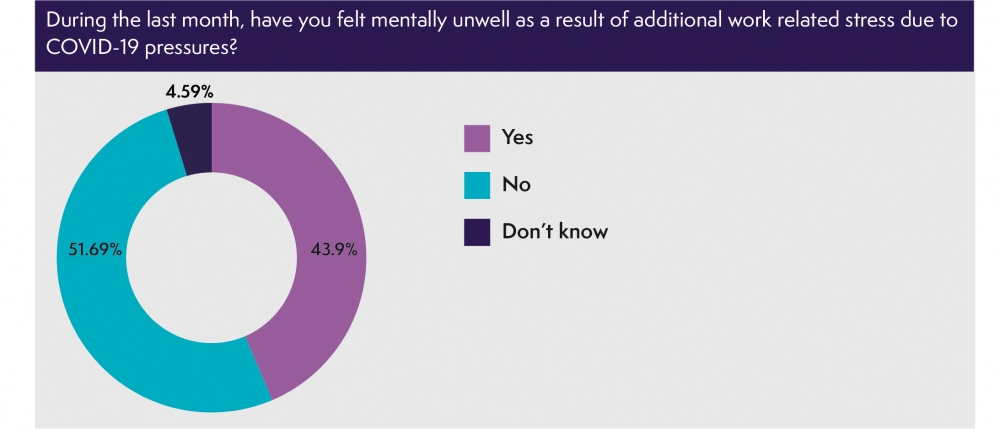
- During the past month, over 40% of respondents have felt mentally unwell as a result of additional COVID-19 related stress, while over a third have felt physically unwell.
Executive Summary
1. Personal Protective Equipment (PPE) – The surgical and critical care environments place anaesthetists at high risk of aerosolised transmission of viruses. PPE forms a critical part of safe working for anaesthetists who need enhanced protection and are in prolonged close contact with symptomatic or vulnerable patients. That’s why 71% of those surveyed told us that access to acceptable PPE is their top priority. Its absence puts lives at risk. Not just those of our members who, alongside other front-line healthcare workers are leading the fight against COVID-19, but those at home to whom they return after their long shifts at hospital.
The cross-government UK-wide COVID-19 PPE Plan will help to ensure that PPE is delivered to those on the frontline.1 However, at time of writing, over two thirds of anaesthetists (73%) told us they feel concerned for their health because of a lack of adequate PPE, with nearly one third (28%) very concerned. With nearly 17% still unable to access the PPE they need, it is easy to understand their apprehension. In this situation, it is of concern that over one quarter of our members currently feel to some degree, pressurised to treat patients without adequate PPE.
Updated PPE guidance was published by Public Health England (PHE) on 17 April 2020. PHE stated that the guidance is aligned with World Health Organization advice on PPE use during “severe shortages” and the US’s Center for Disease Control and Prevention on “crisis capacity strategies”. The College is concerned by the UK Government’s assessment that PPE supplies are becoming inadequate; and is further concerned by the lack of evidence that the new guidance provides equivalent protection to recommendations previously published.
“If this becomes an issue in the future, I will not be treating anyone with COVID-19 without the correct level of PPE – or expecting anyone else on the team to.”
We have to consider whether these updated recommendations represent an erosion of PPE standards. PPE shortages mean those delivering care to NHS patients may have to make difficult decisions, balancing the safety of patients against their personal safety and that of other staff, those they return home to after work and future patients. The College’s first responsibility is to patients and to our members who care for them. We support our members in acting in compliance General Medical Council guidance on decisions as to whether or not to provide care faced with a particular set of circumstances.2
2. COVID-19 testing – the Government’s commitment to increase testing capacity to 100,000 tests every day by the end of April is vital to developing a greater understanding of the scope of the infection.3 We further welcome NHS England’s confirmation that the testing offer will be expanded to a wider group of NHS staff and household members, including those outside of acute care.4
“The hospital denied my request to do the test despite having mild shortness of breath.”
However, with a limited supply of COVID-19 tests they must be prioritised in a way that best mitigates spread of the disease. And, with 17% of anaesthetists having had to self-isolate because of suspected COVID-19, rising to nearly a quarter (24.1%) when including confirmed cases, the sooner anaesthetists are tested, the sooner those who are negative can return to the frontline, treating their patients and supporting their colleagues.
“We are treating all patients as COVID-19 positive. So, all operations are done in surgical masks and aprons, and suspected and positive patients are intubated with FFP3, visors, gloves, long sleeved gowns. This is undoubtedly slowing our efficiency enormously, impairs communication, and is very uncomfortable.”
Increased levels of testing is the second highest priority that our members have told us about (58%), after PPE. In this context, we underscore that at time of writing, almost four in ten anaesthetists (38%) are currently unable to access the testing they need for themselves, while more than half (51%) don’t have the testing they need for household members, and over one in five (22%) are unable to access the testing they need for their patients.
3. Supply of anaesthetic drugs – Various drugs commonly used in anaesthesia are under supply pressure due to increased demand driven by the COVID-19 pandemic. On 2 April, the Secretary of State for Health and Social Care outlined that the Government has a “very detailed plan for making sure that we have the full supply of medicines, including sedatives and all the medicines needed for those who have COVID-19 and people being ventilated.5
The College welcomes the Secretary of State’s confidence that the UK has “the supplies of medicines that are needed”. However, while almost four fifths of anaesthetists are currently able to access the anaesthetic drugs they need, at time of writing more than one in ten (13.7%) do not have access to all the usual drugs; and nearly four in ten (39.1%) are not confident that they will have sufficient supply over the next month.
To manage additional demand, the Royal College of Anaesthetists, Association of Anaesthetists, Faculty of Intensive Care Medicine, Intensive Care Society and UK Clinical Pharmacy Association have worked closely with the Chief Pharmaceutical Officer at NHS England to publish clinical guidance summarising potential mitigations.6 Departments of anaesthesia and intensive care are currently collaborating with each other and with pharmacists to ensure drugs are prioritised appropriately across the two areas.
4. Urgent and acute, non-COVID-19 patients – The NHS has redirected staff and resources, with Trusts postponing “all non-urgent elective operations from 15 April at the latest for at least three months”.3 As intensive care capacity has increased, many anaesthetists have been redeployed into ICUs and, in the last month, four in ten (42.86%) have worked outside their usual area of practice.
The College has concerns about the effect of this on non-COVID-19 patients, e.g. cancer patients requiring acute treatment. It is critical that anaesthetists continue to deliver care to these patients throughout the pandemic. We would welcome greater clarity on existing and future non-COVID-19 demand, e.g. how and where it will be managed, and how resources such as drugs, ICU beds and anaesthetic machines will be shared for non-COVID patients. Thought should be given to how and when some anaesthetists can be redeployed back to anaesthesia from ICU, e.g. with support from other cross-skilled trainees and consultants.
Capacity planning and oversight should be flexible and locality based and timeframe focused, while recognising the anticipated national situation. For NHS hospitals, Trusts and Health Boards where local demand may start to outstrip capacity, additional capacity can be accessed through mutual aid between institutions within established regional networks or through national support. Such mutual aid might involve the movement of non-urgent patients between different hospitals or regions, and/or the movement of limited resources, such as ventilators. Spare capacity must be a part of the post-COVID-19 plan.
5. Welfare and wellbeing – It is testament to the vocation of our anaesthetists, and their dedication to put their patients first, that under such intense pressure nearly half (45.39%) perceive morale within their team as ‘high’ or ‘very-high’. This also speaks to the way in which anaesthetists are working together as part of multidisciplinary teams. And, it speaks to how well anaesthetists feel their mental health at work is being supported, with over two thirds (66.54%) rating the support they are currently receiving as ‘high’ or ‘moderate’.
However, patient safety depends on our clinicians’ wellbeing. Sustaining this level of morale will be dependent on continuing to ease the strain COVID-19 is putting the NHS under. Over one in ten anaesthetists (13.71%) are currently at risk of burnout, while over two thirds are under a high degree of pressure. One-third (33.98%) have felt physically unwell, and four in ten (43.9%) mentally unwell, during the last month as a direct result of COVID-19 stress.
In the short-term, there are clear implications for the morale and welfare of staff (including executive teams), who will need a package of support now, during the pandemic, and post-COVID-19, including adequate leave to rest and recuperate, and access to an appropriate level of mental healthcare and support. The College is further concerned about the risk that some clinicians may suffer PTSD in the months following COVID-19 pandemic. There has been increased access for psychological and mental health support across many sites (supporting healthcare workers) during COVID-19. These will need to be maintained after the crisis.
“Longer and more shifts are making me physically and mentally exhausted to the degree I often think of resigning”
However, pre-COVID-19, our anaesthetists and health and care colleagues already faced a number of workforce pressures that the pandemic has amplified. The health and care landscape must change significantly. In the aftermath of COVID-19 there will be a chance to reflect, and to design a truly 21st century model of care for our National Health Service that best serves our patients and staff. We will need to address staff shortages, redesign and reduce pressure on primary, secondary and social care, breaking down barriers so that we can deliver more personalised, multidisciplinary care based on Shared Decision Making.
“The real impact on staff mental health is likely to occur at the end of this. To be expected to go back to normal working will be unfair.”
COVID-19 clinical guidance hub
Working in collaboration, The Faculty of Intensive Care Medicine, Intensive Care Society, Association of Anaesthetists and Royal College of Anaesthetists have developed a new clinical guidance hub to provide the UK intensive care and anaesthetic community with information, guidance and resources required to support their understanding of and management of COVID-19. Nearly 70% of members are aware of the guidance hub, and over 60% are already finding it helpful in supporting their clinical practice during this crisis.
For more information, please contact
Mark Weiss, Head of Policy and Public Affairs, mweiss@rcoa.ac.uk
