Risks and side effects – chest infection
About this leaflet
This leaflet is about the risk of getting a chest infection after a general anaesthetic. This is a side effect that you might experience if you have a general anaesthetic. The leaflet explains the causes of a chest infection and what can be done about it.
General anaesthetics are medicines that give a deep sleep-like state. They are essential for some operations and procedures. During a general anaesthetic you are unconscious and feel nothing.
You can read about different types of anaesthetics in our Patient information leaflets and video resources section.
What is a chest infection and why it can happen after surgery?
Coughing removes phlegm from your lungs. Phlegm is the mucus in your lungs and chest.
General anaesthetics can affect the way in which phlegm moves from the lungs.
Some operations make it painful or difficult to cough.
If you cannot cough and remove phlegm easily, it can build up in your lungs and infections can develop. For example, pneumonia is a type of chest infection.
How likely is it to happen?
You are more likely to get a chest infection, and need more care afterwards, if:
- you have a long-term illness or are very poorly before your operation
- it is difficult for you to cough effectively after surgery, for example, if you are having surgery on your abdomen (tummy) or you have limited mobility
- you are a smoker.
Out of every 100 people with these risk factors
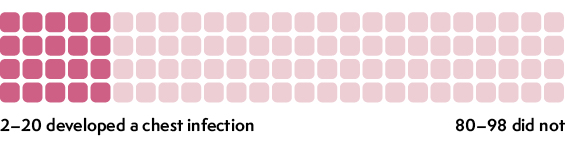
These numbers come from research studies. You can find out about the research we used in our Anaesthesia and risk evidence table.
What if I get a chest infection?
The team looking after you will do some tests to see whether you have a chest infection and what is causing it.
You might find it hard to breathe with a chest infection. The team looking after you will help you if this happens. For example, they can give you oxygen through a mask.
You might have chest or back pain and feel very tired.
Sometimes your blood pressure can fall and your heart beats faster. Your team will monitor your blood pressure and heart rate.
How is a chest infection treated?
There are various things that the team looking after you can do to treat a chest infection.
Antibiotics
Chest infections can be caused by bacteria or a virus. If your infection is caused by bacteria your doctors can give you antibiotics. Antibiotics can be given via:
- a cannula (‘drip’), a very thin plastic tube that goes into your vein
- tablets that you swallow.
Intravenous fluids
Your team can give you fluids through a cannula directly into your vein. These help to soften phlegm in your lungs so that it is easier to cough up. This can also help fight the infection.
Oxygen
Sometimes you can have oxygen through a facemask or small plastic tubes in your nostrils. Oxygen can be quite noisy and make your mouth and nose dry.
If your infection is very severe, you may need to be looked after in an intensive care unit or a high dependency unit. A machine (a ventilator) can help you breathe if needed. You will be sedated if you need this machine.
Physiotherapy
The team might refer you to a physiotherapist who will show you how to breathe and cough more effectively to get rid of phlegm.
What can help prevent it?
If your anaesthetist thinks that you might be at risk of developing a chest infection, they will talk to you before the operation. They will discuss the following with you:
- how likely you are to develop a chest infection after surgery
- whether a different kind of anaesthetic is suitable for you, for example, a regional anaesthetic
- whether you might need extra care after surgery to reduce your risk of developing a chest infection. For example, you might need additional pain relief or physiotherapy to help your breathing.
What can I do myself?
Before the operation
If you are offered a flu vaccine, you should consider taking it because this can reduce the risk of a chest infection.
If you smoke, try to quit six weeks before going into hospital. If you cannot quit, it’s important that you try to stop in the days before your operation. This gives your lungs time to recover from the smoke damage and make them more resistant to infection.
Help is available on the NHS website and via the Centre for Perioperative Care.
After the operation
If you are in pain after surgery, let the team know straight away. They can give you enough pain relief to help you breathe deeply and cough more easily.
You will be encouraged to drink fluids. This can help to make the phlegm in your lungs softer and easier to cough up.
Do any exercises that your team has given you to help you breathe and cough effectively after surgery.
This leaflet has been produced by Leila Finikarides for the RCoA, in collaboration with patients, anaesthetists and patient representatives of the RCoA.
Disclaimer
We try very hard to keep the information in this leaflet accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this leaflet as a guide. This leaflet on its own should not be treated as advice. It cannot be used for any commercial or business purpose. For full details, please click here.
Sixth Edition, November 2024
This leaflet will be reviewed within three years of the date of publication.
© 2024 Royal College of Anaesthetists
This leaflet may be copied for the purpose of producing patient information materials. Please quote this original source. If you wish to use part of this leaflet in another publication, suitable acknowledgement must be given and the logos, branding, images and icons removed. For more information, please contact us.