View from the frontline of anaesthesia during COVID-19, May 2020 survey results
View from the frontline of anaesthesia during COVID-19
Over a 24-hour period from 13-14 May 2020, the College conducted a survey to develop a snapshot ‘view from the frontline’ of anaesthesia during COVID-19.
Introduction
Anaesthetists of all grades play a critical role in the care of patients affected by COVID-19. 1,496 RCoA members from across the UK completed the second in our series of monthly 24-hour snapshot surveys aimed at producing a detailed picture of the issues faced by anaesthetists during this challenging time.
As well as presenting the latest findings, this briefing offers a comparison with the benchmark set through our first survey1 to understand how the pressure and issues on the frontline is changing through the pandemic. This latest survey also aims to explore new emerging pressures, such as the resumption of planned surgical services and the preparedness of both anaesthetists and anaesthetic departments for this.
Who is this briefing for?
Civil servants, ministers, parliamentarians, College fellows and members, clinical directors, NHS, public health and social care organisations across the UK, our partners, and the public.
What is this briefing for?
- To represent the voice of the College’s members on the issues that matter most to them during COVID-19, and to feedback their views as expressed in the COVID-19 survey. To support civil servants, ministers, parliamentarians and key decision makers to understand, and mitigate, the pressures faced by anaesthetists during COVID-19 as they care for their patients.
- To highlight the indispensable role of anaesthetic teams in treating patients with COVID-19, and to encourage decision-makers and the public to champion the profession.
Key findings
-
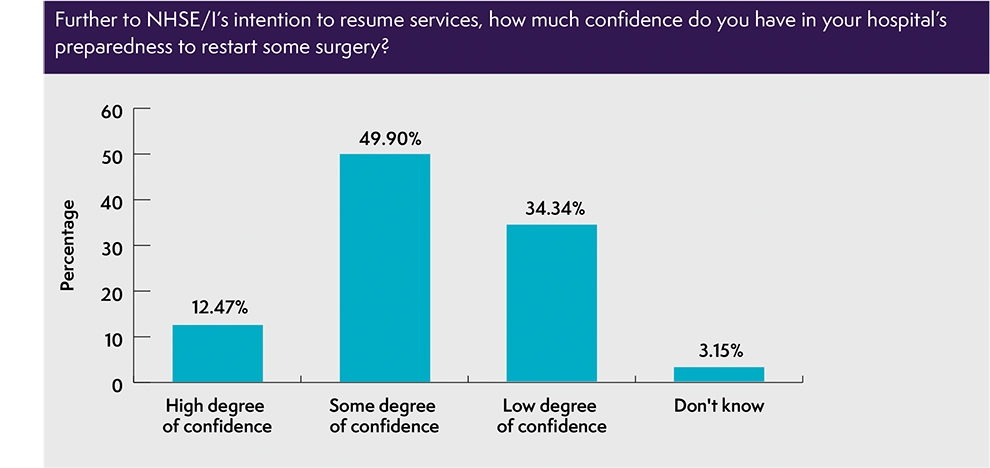
Over a third (34%) of respondents have a low degree of confidence in their hospital’s preparedness to restart some planned activity.
-
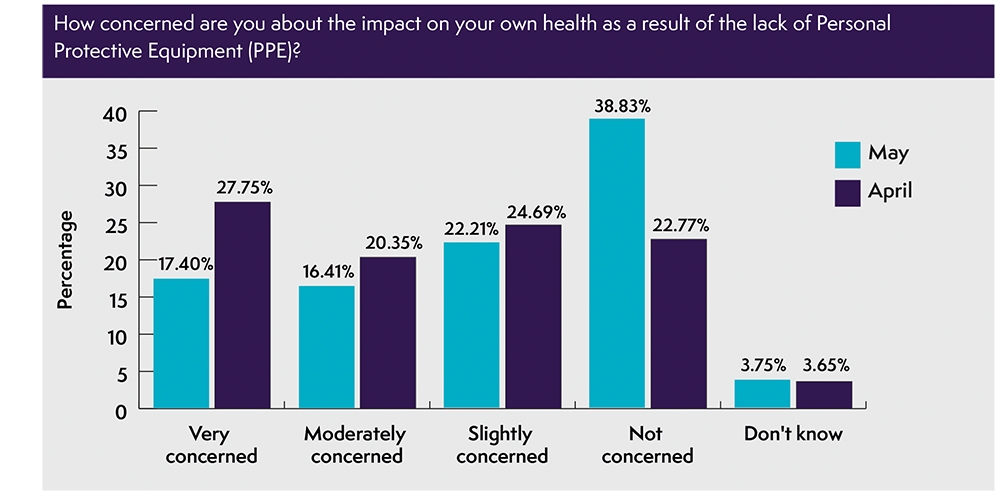
Over half (56%) continue to feel concerned about the impact on their health from a lack of PPE (with nearly one fifth very-concerned, 17%). Nearly one in ten (9.8%) still aren’t confident that they can access the PPE they need, and over one in ten (12.5%) are still delaying patient care due to a lack of PPE.
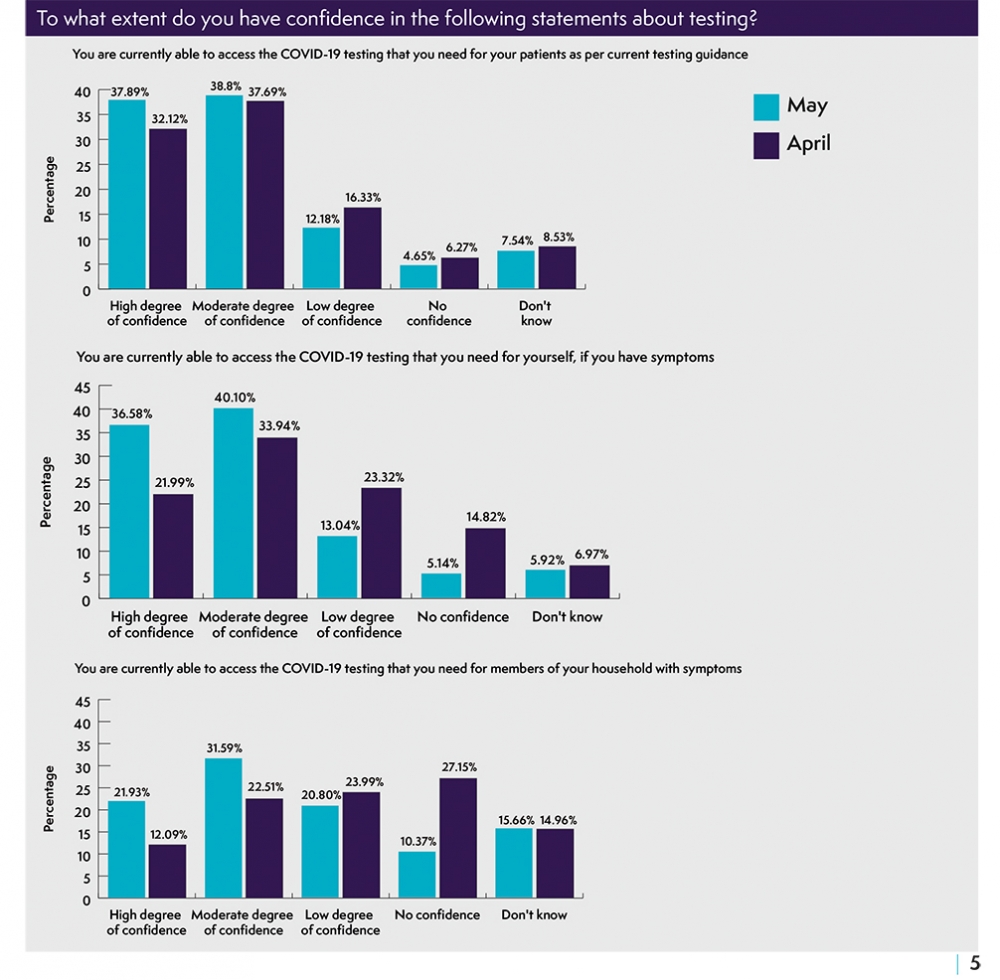
- More than one in six (17%) continue to have a low or no degree of confidence in their ability to access the testing they need for their patients, rising to nearly one in five (18%) when considering access to testing for themselves, and rising again to nearly one third (31%) when considering access to the testing they need for members of their household with COVID-19 symptoms.
- Over one in ten (13%) are still unable to access the anaesthetic drugs they need, while over one in four (27%) are still not confident they will be able to access the anaesthetic drugs they need over the next month.
- More than one in four (42%) reported feeling mental distress over the last month, while over one in ten (12%) feel at risk of burnout.
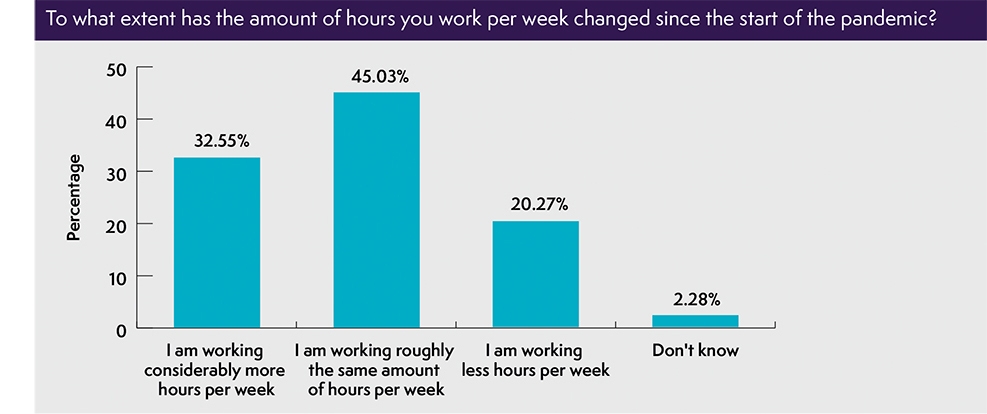
- Nearly one third (31%) of respondents reported difficulties taking annual leave during the pandemic, despite nearly one-third (32.5%) working considerably longer hours.
Executive Summary
One month on from our first survey, the new findings reveal that some progress is being made towards the availability of testing, PPE and anaesthetic drugs. However, our members are telling us that they continue to be concerned about long term availability and accessibility of the resources and equipment they need. The ability of their hospitals to resume planned activity depends (not exclusively) on the short, medium and long-term sustainability of anaesthetic and critical care drug stocks, staffing numbers, personal protective equipment (PPE) and testing capacity.
The second survey also reveals the sustained toll that the pandemic peak has taken on the mental and physical resilience of anaesthetists and their teams. Our members and their health and care colleagues need sufficient time to recuperate before returning to their routine clinical duties.
The findings from our surveys have highlighted how the pressures already faced by our members pre-COVID-19 have intensified during the peak of the pandemic. In the aftermath there will be a chance to reflect, and to design a truly 21st century model of care for our health and care service that best serves our patients and staff. There is a need to address staff shortages, service redesign and reduce pressure on primary, secondary and social care in the context of integrated care. The setting up of a time limited Investment and Transformation Fund could support the development of perioperative care pathways that break down barriers and facilitate the delivery of more personalised, multidisciplinary care based on Shared Decision Making principles.
1. Preparedness to resume routine anaesthetic services – The impact of COVID-19 on service delivery will be sustained for many months. Management of both COVID-19 demand and resumed activity will therefore require additional investment in staff, resources and critical care capacity, against an underlying principle that all patients across the UK should have equity of access to treatment. It is vital that standards of patient and staff safety are not compromised by a determination to increase productivity in an effort to ‘get back to normal’.
The Royal College of Anaesthetists, in collaboration with the Faculty of Intensive Care Medicine, the Intensive Care Society and the Association of Anaesthetists, has produced a strategy document offering guidance on how planned activity can be resumed safely, efficiently and in a sustainable manner, taking into account the staffing, environment and equipment needed.2 The strategy outlines, and ‘RAG-rates’, a set of criteria to be met across four broad areas (space, stuff (equipment), staff, and systems) before elective activity is resumed, including (but not exclusively):
- Sufficient numbers of staff should be available to return to their routine work.
- Sufficient anaesthetic and critical care drug stock levels should be secured.
- Sufficient supply of PPE (and access to it) should be available.
- Temporary ICUs in key locations within the surgical pathway should be evacuated or relocated.
- All Standard Operating Procedures for surgical services, theatres and critical care should be reviewed and, if necessary, adjusted.
In the context of the publication of this four organisation strategy, and The UK Government’s own COVID-19 recovery strategy and ‘Plan to Rebuild’3 , we asked our members how prepared they feel their departments are to resume anaesthetic services. Whilst almost half of respondents feel mentally and physically capable of returning to planned activity, over a third (34 %) told us that they currently have a low degree of confidence in their hospital’s preparedness to restart some planned activity.
“Our main stumbling blocks to restarting elective work are availability of drugs and sufficient PPE”
Reassuring patients and the public on the importance of attending hospital appointments and surgical procedures by communicating to them the steps that healthcare staff are taking to keep them safe is a critical part of resuming surgical services.
The Centre for Perioperative Care has published an FAQ to address some of the concerns that patients may have about going to hospital during the pandemic and offering advice on the importance of preparation for surgery and shared decision making at this worrying time. The FAQ document complements the NHS’ Operating framework for urgent and planned services within hospitals.
2. Personal Protective Equipment (PPE) Supply of PPE remains our members’ number one priority issue. We therefore welcome the Government’s commitment to “engage in a massive plan to ramp up domestic supply of PPE”.
While there has been a decrease in the number of respondents who are to some degree concerned about the impact on their health from a lack of PPE (down 17% from last month), over half (56%) continue to feel concerned (with nearly one in five very-concerned). Nearly one in ten (9.8%) still aren’t confident that they can access the PPE they need, and over one in ten (12.5%) are delaying patient care due to a lack access to PPE. In this context, it is of concern that at the time of writing more than one in five (22%) continue to feel some degree of pressure to treat COVID-19 patients without adequate PPE.
“As time passes I am concerned there will be problems in supply further down the line”
The availability of high quality PPE will be an essential element of the NHS’ ability to resume surgical services and to maintain the safety of both patients and staff. A consistent and reliable supply of the PPE needed for the management of hospital patients throughout the pandemic must be available before resuming any planned activity.
3. COVID-19 testing – It is heartening to see that the Government’s commitment to meet its testing target of 200,000 a day by the end of May is translating into improvements for our members on the ground. Nearly four in five (76.66) now have a high or moderate degree of confidence that they can currently access the testing they need for their patients.
Our members also tell us that there has been an improvement in their ability to access tests for members of their household (20% more than the previous month).
Adequate testing for patients is a critical component of the NHS’ plans to resume planned activity. The Operating framework for urgent and planned services in hospital settings during COVID-19, outlines the requirement for all patients to be tested for COVID-19 prior to admission, for testing to be repeated regularly for patients admitted for longer periods and for patients discharged to care homes to be tested before leaving hospital.
Despite progress made, the College remains concerned that more than one in six (17%) members responding to the survey continue to have a low, or no degree of confidence in their ability to access the testing they need for their patients. This rises to nearly one in five (18%) when considering access to testing for themselves, and rises again to nearly one third (31%) when considering access to the testing they need for members of their household with COVID-19 symptoms.
Availability of testing is particularly important in supporting the more than one in ten anaesthetists who continue to be taking time off from their normal work schedule due to suspected COVID-19 (either themselves or members of their household) to return to work, so that they can support their patients and colleagues.
As the Government eases the lockdown over the coming weeks and months, health and care staff, and the patients they care for, must have confidence in the UK’s approach to testing, tracking and tracing, including the accuracy of testing, based on an integrated and comprehensive plan to mitigate the risk of a second surge in COVID-19 infections.
“Concerned about the second wave in view of too early easing of lockdown by government without adequate testing facilities to track and trace infected people”
4. Supply of anaesthetic drugs – The Government’s acknowledgment, on 28 April, that “there is an increase in demand for a number of intensive care drugs including anaesthetic drugs”, and commitment to do “everything [it] can to ensure patients continue to access safe and effective medicines” is welcome.5 We are also grateful to NHS England and the Chief Pharmaceutical Officer for their transparent and regular engagement with the College and our partners on this vital issue.
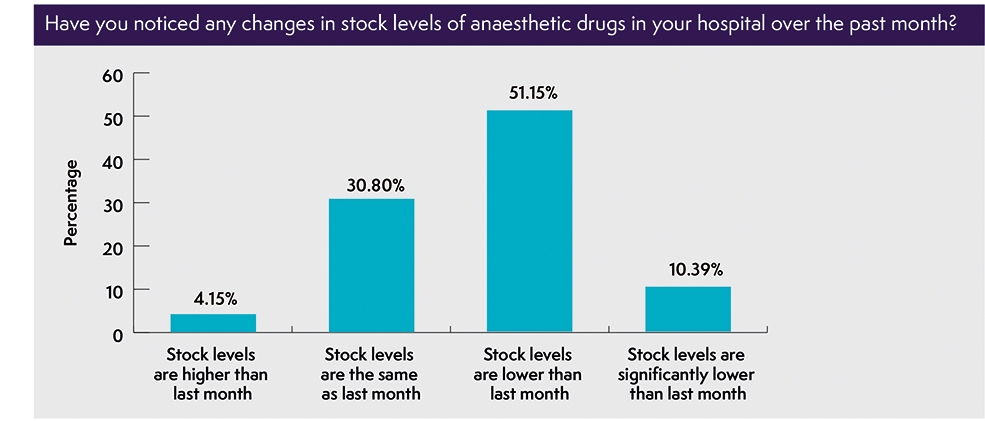
While it is encouraging that our members’ confidence has improved in the future supply of anaesthetic drugs, one in four respondents (27%) continue to be concerned at their ability to access the drugs they need over the next month. Over 50% reported that they have noticed a drop in drug stock levels over the past month, while over one in ten (126%) continue to be unable to access the anaesthetic drugs they need (only a small change from the previous month (13.7%).
“I feel trepidation mainly around the drugs I am most comfortable with not being available”
To manage additional demand of anaesthetic drugs, the Royal College of Anaesthetists, Association of Anaesthetists, Faculty of Intensive Care Medicine, Intensive Care Society and UK Clinical Pharmacy Association have worked closely with the Chief Pharmaceutical Officer at NHS England to publish clinical guidance summarising potential mitigations.6 Departments of anaesthesia and intensive care are currently collaborating with each other and with pharmacists to ensure drugs are prioritised appropriately across the two settings.
5. Welfare and wellbeing – The safety of patients, both COVID and non-COVID, depends on the mental and physical wellbeing of our anaesthetists. One month on, the findings from our latest survey reveal that there has been little improvement in the welfare and wellbeing for anaesthetists on the frontline. Over one in ten (12%) continue to feel at risk of burnout, while over four in ten (42%) have felt mental distress during the last month as a direct result of additional work related stress due to COVID-19, and almost a third have felt physically unwell.
Nearly one third (32.5%) report working considerably longer hours during the pandemic. Our members are adapting to a considerable change in working patterns during the pandemic peak, with many more feeling the strain of being on call more frequently, and from working nights and longer shifts.
“The pattern of work has changed completely”
These sustained pressures are also taking their toll on morale. One in five (20.82%) perceive morale in their team to be either low or very low. Anaesthetists who have been heavily involved in the management of the most serious COVID-19 cases during the peak of the pandemic need adequate rest to recuperate before going back to routine clinical duties and must be allowed to take leave.
“Feeling exhausted and aware that colleagues are starting to feel frayed by all that has happened and relationships are under threat, despite what has been a very collaborative approach up to now.”
The increase in unsociable working hours will have an effect on the wellbeing of anaesthetists and their work-life balance. The College remains concerned about the risk that some clinicians may suffer PTSD in the weeks and months following the COVID-19 peak and calls for the maintenance of mental support services throughout the pandemic, such as those highlighted by the British Medical Association.
“I’m tired. The thought of doing more work in hot/sweaty PPE is overwhelming.”
As outlined in the four organisation strategy for the restoration of planned activity, any movement towards restoration should be based on an acceptance and remediation of:7
- the potential for fatigue/stress from shift working patterns, long hours and dealing with death
- accumulated time owed for Bank Holidays and annual leave
- sickness resulting from coronavirus or other illnesses
- inadequate access to educational activities compliant with normal revalidation requirements
- unremunerated clinical time owed for flexible working patterns under surge conditions.
Anaesthetists of all grades have played an indispensable role in the management of the pandemic. Their ability to quickly redeploy and adapt their working practices to support intensive care colleagues is testament to their unique skill set. Planning for possible future COVID-19 surges, pandemics and other pressures requires reserve capacity and flexibility in the system, and should embed a sustainable, and adequately staffed, anaesthetic workforce to fully support the health and care service to cope in times of crisis and beyond.
COVID-19 clinical guidance hub
Working in collaboration, The Faculty of Intensive Care Medicine, Intensive Care Society, Association of Anaesthetists and Royal College of Anaesthetists have developed a clinical guidance hub to provide the UK intensive care and anaesthetic community with information, guidance and resources required to support their understanding of and management of COVID-19. There is a growing awareness and use of the guidance hub. Over 70% of members are now aware of the guidance hub, and over 60% continue to find it helpful in supporting their clinical practice during this crisis.
For more information please contact:
Elena Fabbrani, Policy and Patient Information Manager, efabbrani@rcoa.ac.uk
